The Walking Child
Orthopedic intervention is often required to either improve or maximize walking ability or to preserve it. The growing child often requires significant compensatory movement in order to ambulate with or without the assistance of crutches or walkers. Due to limited strength and weight during adolescence this abnormal, compensatory motion becomes more difficult to perform. This may result in walking limitations and even the requirement of a wheelchair.
Toe-walking
Toe-walking is one of the earliest manifestations of cerebral palsy. The increased tone/spasticity in the calf muscle leads to the child walking on his or her toes. Toe-walking can be detrimental to the structures of the foot themselves and can often result in a breakdown of the midfoot and flattening of the arch. Initially treatment is focused on stretching, Botox injections, and braces such as an ankle-foot orthoses (AFO). Surgical treatments include lengthening of either the muscle or tendon of the calf to improve their walking capacity and eliminate the chance of further midfoot breakdown.
Hemiplegic Gait
A child with a hemiplegic-type gait pattern with unilateral spasticity often walks on their toe with progressive knee and hip flexion contractures, resulting in a functional shortening of the leg and an abnormal gait. Once again, bracing and Botox injections along with physical therapy are the initial treatment options. However, if these fail, the child may require surgical lengthening of the muscular tissue or tendon tissue of the calf, knee, and possibly hip. During growth spasticity provides additional abnormal muscular forces on the growing bone of the lower extremity causing torsion or twisting deformities to the foot, thigh bone (femur), and leg bone (tibia). When these conditions occur, in order to restore appropriate alignment and maximize gait, bony incision and correction of the long bone and foot deformities may be required.
Diplegic Gait
A child with a diplegic gait often displays a crouched gait pattern. Essentially progressive deformities arise due to spasticity, muscular contractures, and developing bony deformities affecting alignment, strength, and what is commonly called lever-arm disease. The ankle is usually rolled out with the foot out-toeing which may cause severe flat feet. This leads to buckling in at the knees and external rotation deformities of the legs (tibia). Additionally, rotational deformities of the femur (thigh) as well as hip flexor contractures are also observed. This results in a child falling forward in a partial squatting position unable to stand up fully struggling to ambulate. When the child progresses to a crouched gait pattern he also requires surgery in order to re-lengthen contracted muscle and tendon structures, realign bony deformities, and correct the significant planovalgus (severe flat feet) foot deformity. As with the majority of the procedures performed on a child with cerebral palsy, rapid and aggressive physical therapy is additionally required in a motivated child to establish optimal benefits.
Sitting (Non-Ambulatory) Child
The child who has never achieved the ability to walk also requires orthopedic assessments and possible intervention to achieve appropriate sitting balance and avoid future pain and deformity. While soft tissue lengthening, specifically at the ankle, may be necessary for wheelchair positioning, the majority of procedures in the sitting child are focused on the child’s hips and spine.
Hip Dysplasia (Hip Dislocations)
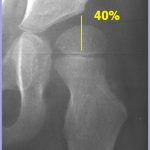
Children with spastic quadriplegia have severe abnormal forces of the hips, specifically in adduction and flexion, often resulting in migration of the hip out of the socket joint. These children develop this condition pre-adolescent and usually without pain. However, the majority of these children develop pain as an adolescent and into adulthood causing sitting intolerance and diminished quality of life. Initially, if a child is quite young and the hip has not fully dislocated, consideration of simple adductor tendon release (tendon/muscle of the inner thigh) can result in reduction of further progression of the deformity. When the child is within the optimal years of age (6-12 years) reconstructive procedures Varus Derotational Osteotomy(VDRO) are performed to reduce the head into the socket and stimulate normal development of the hip joint. Varus derotational osteotomy – An incision into the bone of the initial 1/4 of the femur in which rotation and angular correction of the bone is achieved with a hip plate and screw fixation to realign the ball of the femur into the alignment of the socket joint. However during the adolescent years further deterioration of the dislocated hip occurs eliminating the ability for reconstruction. While not optimal, procedures (resectional arthroplasty or removal of the hip joint versus partial replacement or hemiarthroplasty) exist in these situations for pain relief. Iliac osteotomy – Once the ball joint is replaced into the socket joint, the socket joint is reconstructed in order to capture the head of the femoral head (ball) more effectively by lowering the roof of the socket.
Scoliosis & Spinal Deformities
Scoliosis (twisting angulation of the spine) and kyphosis (forward bending of the spine) are quite common in the spastic child and are involved in 70% of children with spastic quadriplegia. The deformity is not present at birth, but develops during growth of the child. Typically the curve requires intervention if it progresses beyond 40 degrees and/or the pelvis angles obliquely so that the child has difficulty with sitting. Progressive scoliosis not only leads to sitting intolerance, but in the quite severe conditions may lead to cardiopulmonary compromise and become life threatening. Bracing has not shown to be significantly effective in correcting or halting the progression of neuromuscular scoliosis as it is in idiopathic scoliosis. However, it may maintain the child more erect in a sitting position. Wheelchair modifications can lead to the same results, without resulting restrictive respirations that may occur with brace wear. However, once the curve becomes quite severe, surgical intervention is the only effective treatment. While the procedure is not minor, it can be performed safely and effectively in restoring spinal balance, even in the significantly involved child. The procedure requires instrumentation(metallic screws, wires and hooks) to be placed into the bony structures of the spine (vertebrae), which act as fixation points for which the spine can be manipulated. Rods are then connected to the fixation points on each side of the spine, maintaining the correction.
Upper Extremity
Children with severe cerebral palsy often have contractures of the upper extremities limiting function, range of motion, and access for hygiene and care. Contractures can range from mild elbow limitations in extension to severe flexion deformities of the thumb, wrist, elbow, and shoulder.
Children under the age of 6 years old are usually treated conservatively by means of:
- Occupational therapy for gross motor coordination.
- Encouragement to use both hands during play.
- Nighttime splinting and bracing.
The care of children between the ages of 6-12 years of age focuses on more aggressive treatments such as:
- Fine motor skills and activities of daily living.
- Botox injections for dynamic contractures.
- Surgical consideration for fixed contractures.
- Functional gains with surgical intervention are dependent on:
- Voluntary control.
- Upper extremity sensibility.
- Intelligence with an IQ greater than 70.
- Neurological type and severity.
- Functional gains with surgical intervention are dependent on:
Upper extremity treatment of an individual with cerebral palsy greater than 12 years of age focuses on activities of daily living. At this age there is a consideration of assisted technology. As the child grows older he/she becomes less able to adapt functional ability and thus unable to improve with surgical modifications. Surgery to restore function at this age group is less predictable and may be difficult. However, surgery may improve cosmesis. The appearance of the extremity to the adolescent is important and should not be under appreciated.